You may already be ordering germline testing at rates well above the national average — but across the U.S., most eligible patients still aren’t tested:
- Ovarian cancer: ~39% receive germline testing
- Pancreatic cancer: <20% tested
- Metastatic prostate cancer: ~30% tested
- Breast cancer ≤65y: ~26% tested
These aren’t “screening” tests.
Germline results are therapeutic biomarkers — guiding PARP eligibility, platinum use, surgical planning, immunotherapy access, and cascade prevention. When testing is missed, treatment is lost.
Why Even High-Performing Practices Face Friction
Even in programs with strong adoption, systemic barriers remain:
- Insurance and billing delays in cascade testing
- Limited counselor capacity for the volume of positives
- EHR workflows that don’t flag edge cases
- Drop-off when multiple handoffs are required
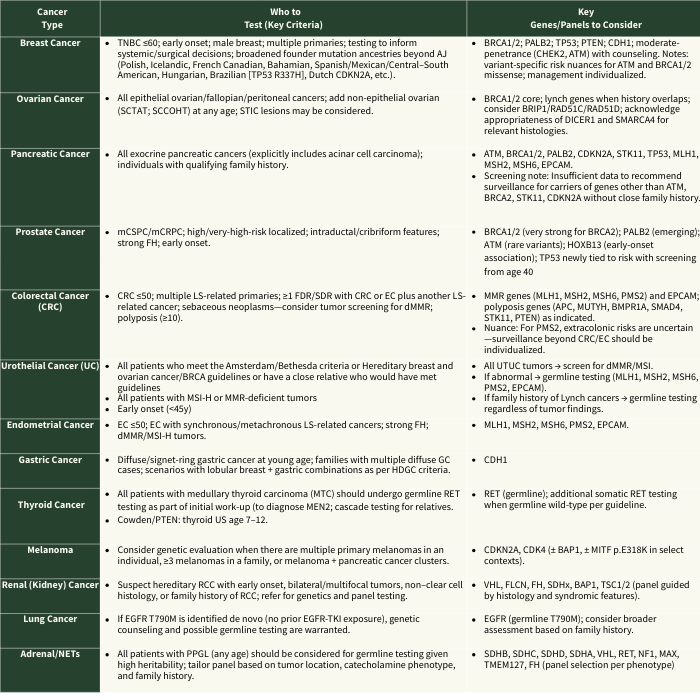
NCCN Germline Testing Triggers at a Glance
📌 Download Summary Table and Potential Clinical Implications Here
For quick reference, here are the core guideline sources:
1. NCCN Genetic/ Familial High-Risk Assessment: Breast, Ovarian, Pancreatic, and Prostate
2. NCCN Genetic/ Familial High-Risk Assessment: CRC, Endometrial, and Gastric
What the Best Centers Have Proven Works
- Mainstreaming (Kaiser Permanente): EHR-embedded, diagnosis-triggered orders → doubled uptake, cut turnaround times.
- Point-of-Care (Duke): Testing at check-in and same-day completion → tripled uptake, disparities erased.
- Embedded Counselors (City of Hope, Texas Oncology): Onsite navigators and nurse-led intake → 91% uptake; 70% of results altered management.
These aren’t pilots — they’re scalable, repeatable systems.
The Opportunity for Leadership
For community leaders, the next frontier isn’t whether to test — it’s system design: workflows that push uptake toward 90–100% while protecting patients and families from preventable harm.
One often-overlooked safeguard: when cascade testing relatives, confirm insurance coverage for life/disability before ordering. Otherwise, well-intentioned prevention efforts can backfire into avoidable financial exposure.
If your center is already close to universal testing, you’re modeling the future of cancer care. The challenge now is scale: extending what works in your practice across networks and into the broader community.
Bottom Line
This isn’t about awareness anymore. It’s about design.
If your ovarian, pancreatic, or metastatic prostate cancer patients aren’t universally tested, it’s not a gap — it’s a solvable systems problem.
I hope you find this summary of trigger guidelines and proven workflow models useful as you evaluate your current processes and identify opportunities for improvement.
—————————————
The Compass is your practical briefing on what’s working in oncology care – strategy, science, and systems. No fluff. Just implementation.