The most precise cancer therapy means nothing if the patient declines it.
That’s not a failure of medicine – it’s a failure of transmission.
Patients now arrive with TikToks, chatbot printouts, and “cure” stories from forums. Some are skeptical, others scared—but nearly all are primed before they ever hear your plan. The result: delayed treatment, trial attrition, and refusal of guideline-based care.
A 2025 UF Health study found that 93% of newly diagnosed patients encountered cancer misinformation – often without searching for it. Social feeds, relatives, and YouTube thumbnails now shape belief faster than any consult can correct.
Your patients are smart and curious, trying to make sense of their diagnosis – but the system around them is engineered to mislead. The effect is measurable: patients influenced by misinformation are less likely to start or stay on evidence-based therapy, directly affecting survival
Quantifying the cost of misinformation exposure
- Patients with low health literacy have a 9.4‑month shorter median survival, independent of stage or access to care.
- Choosing unproven alternative therapies instead of evidence-based treatment increases mortality risk two‑ to five‑fold in curable cancers
- Younger patients (Gen Z) increasingly rely on influencers for medical decisions and often rate their trust in these sources as higher than in physicians
This isn’t just a communication problem – it’s a risk factor hiding in plain sight.
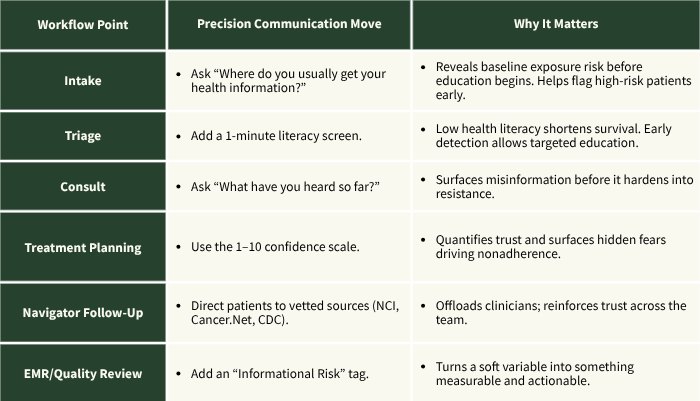
Turning Everyday Conversations into Scalable Precision Communication
You’re likely already doing this: spending extra minutes re‑explaining basic biology, listening through layers of internet influence, and bringing the discussion back to evidence. The shift? Stop treating that as a workaround – and start treating it as part of the care plan.
Three high-impact moves that require no new infrastructure:
- Surface the source early
“What have you heard about this treatment so far?”
This quickly identifies exposure and frames the conversation around it. - Use the confidence scale
“On a scale from 1–10, how confident are you in our plan – and what’s keeping it from being a 10?”
If the answer is “5, because I read chemo is toxic,” you’ve just diagnosed the real barrier. - Prescribe credible sources
“Here are two sites I trust. Before our next visit, take a look – we’ll review them together.”
Treat misinformation like a nutritional deficiency: identify it, document it, and replace it.
👉 The NURSE mnemonic (Name, Understand, Respect, Support, Explore) by Tulsky et al offers a simple, evidence-based way to communicate with empathy – even about misinformation.
You can’t outcompete social media – but you don’t need to. What matters is framing:
- Not “patients are falling for conspiracy theories,” but “misinformation is an exposure risk – like any environmental toxin.”
- Not “we need to debunk myths,” but “we need a reliable way to identify and respond to informational risk.”
This isn’t about fixing the internet. It’s about embedding communication into clinical workflow – and making it actionable, scalable, and measurable.
Practical steps health systems could explore
Most oncologists didn’t train to battle algorithms. But here we are. The system must now adapt to the information ecosystem patients live in.
The good news? Even when they’re skeptical – even when they arrive with printouts or viral videos – they still show up for you.
You can’t fix the problem yet. But you can name the risk – and own the conversation before someone else does.
——————————————
The Compass is your practical briefing on what’s working in oncology care – strategy, science, and systems. No fluff. Just implementation.